Familial dilated cardiomyopathy
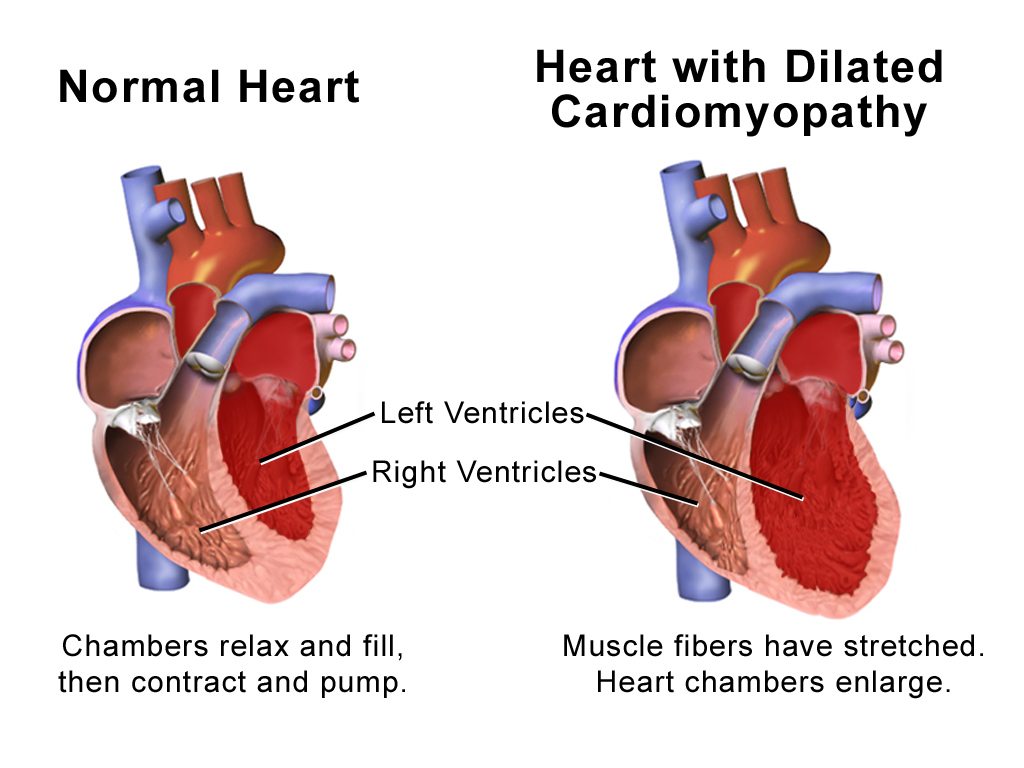
This is usually due to genetic abnormalities in the structure of the heart muscle cells so that they do not function normally. Over time, this can lead to the heart becoming dilated with thin walls and a weak pumping action. If the condition is not detected and is left untreated, heart failure (where people experience shortness of breath, fatigue and swelling of the legs and abdomen) and heart rhythm problems (causing dizziness, fainting or palpitations/forceful heart beats) can occur. It is also possible to have mild disease and no symptoms at all.
Factors which suggest that DCM is familial include: no other cause for the DCM was found (such as coronary artery or valvular heart disease), and there is another family member affected by unexplained DCM. It’s important to note that not everyone with familial DCM presents the same way – some may have heart failure, while others have heart rhythm problems.
Genetics of familial DCM
In familial DCM, there are mutations in over 30 genes which code for the building blocks (proteins) of the heart muscle cells. There are probably many more mutations which cause DCM which science hasn’t found yet. Most commonly, DCM is inherited in an autosomal dominant pattern which means that if a person carries one mutated gene, they are at risk of developing DCM. Both males and females, and young and old people are affected. If someone in your family has DCM (and no cause for it was found), or if someone carries a genetic mutation causing DCM, it means first degree relatives (children, brothers/sisters and parents) have a 50% chance of having risk (not guarantee) of developing DCM. Other patterns of inheritance for DCM occur such as recessive and sex-linked.
Family screening
Therefore, we recommend that family members are screened with an electrocardiogram (ECG, where sticky dots are placed on the chest and abdomen to record the heart rhythm) and echocardiogram (where an ultrasound of the heart is performed to check the size and function of the heart muscle) to see if they are affected or not. Depending on the situation in the family, we may recommend that these tests are repeated every few years. It may be possible to have a predisposition to DCM, or have early disease, but not have any symptoms, and that’s why it’s a good idea to be checked. Detecting DCM early means that a person can take control by making healthy lifestyle choices, and perhaps taking medications to prevent their heart becoming any weaker or more dilated.
Genetic testing
In some families, genetic testing may be possible. We begin with taking a blood sample from someone who definitely has DCM. Their blood is tested for all the gene mutations we currently know about. There are three basic types of results we can get. First, we may not find a gene change – this doesn’t change the fact that the person has DCM, it just means science doesn’t know the particular mutation yet. Second, we may find a “variant” (or a change in the gene where we are not sure if it causes DCM or not). In this situation, we may do some more investigating, and ask other affected family members to see if they also carry the same variant. The third kind of result is where we find a mutation which we are confident causes DCM and in these cases, we can test other family members to see if they are at risk, or not, of developing DCM. Those who don’t have the mutation don’t need to have ongoing screening, and won’t be able to pass on this genetic predisposition to any children they may have.
What to do if you suspect familial DCM
Talk with your cardiologist, or contact us via the website and try to find out information about your family member’s heart conditions. Your family history should be documented thoroughly.
What to do if there is familial DCM
Whilst we can’t change our genetic make-up (yet!), it is sensible to try and maintain optimal heart health. Consult the NZ National Heart Foundation website for tips on managing traditional risk factors for ischaemic heart disease such as your blood pressure, cholesterol and diabetes. Please – quit smoking, and avoid excessive amounts of alcohol.
Encourage your family members to come in for clinical screening, even if they don’t have any symptoms. It may be possible for them to have genetic testing.
If you have familial DCM, it’s important to keep seeing your usual cardiologist. They will make sure you receive any treatment you require, and to make sure your risk of any serious problems is minimized.